…and what they mean to Medicine and Patients
by Tom Grier , Microbiologist
Download pdf version
with extra spacing to aid neuroborreliosis patients.
Page 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10
- Mother-to-child transmission of Borrelia across the womb
- Finding Borrelia burgdorferi and miyamotoi associated with Amyloid Plaques in Alzheimer’s disease brains
- Finding Borrelia in Lewy Body Dementia
- Nematode worms found in the CSF (spinal fluid) of Multiple Sclerosis patients
- Nematode worms found in Alzheimer’s brains
- Borrelia found in five deadly brain tumors (Glioblastoma multiforme)
- Borrelia Mayonii and Borrelia burgdorferi found in human testicle
Since 1975 when Lyme disease was first introduced to the medical literature, it has been surrounded by controversy and misunderstandings. Much of the problem stemmed from trying to understand this disease entirely through antibody tests (serology) based entirely on just one species – Borrelia burgdorferi.
We now know that there are many species of Lyme disease. Borreliosis is not just one disease, it is part of a family of diseases that can no longer be considered separate or isolated from Lyme disease. The best example of this is Borrelia miyamotoi. It is found in hard-shelled ticks just like Lyme disease, but it is a Relapsing Fever borrelia. It took over 10 years for microbiologists to place it in the Relapsing Fever category as opposed to the Lyme-genetic grouping.
Not surprising is the fact that B. miyamotoi is found in the human brain right alongside B. burgdorferi. They may look like two separate diseases on paper, but in the human brain they are pathogens and must be eradicated together.
An even more concerning part of the Lyme disease story is that virtually no funding in any country has been put into Borrelia pathology. The fact is Lyme serology simply cannot detect this family of bacteria with any reliability, mostly because Borrelia, once inside the human brain, is behind the blood-brain-barrier, and inside human brain cells. As a result, the human immune system can no longer recognize it.
Add to this the fact there are more than a dozen species of Borrelia that cause Lyme disease, many of which can penetrate any tissue, and add a couple Relapsing Fevers that tag along for the ride, and it becomes clear that the Lyme disease blood tests based on Borrelia burgdorferi detection that have been used for 30 + years have become pretty much useless.
I first met Dr. Alan MacDonald and Dr. Paul Duray in 1992, and I was excited because they were doing the kind of research that I thought was beneficial, focusing directly on the disease process. Their pathology-based research got to the heart of it. In a sea of endless tick and deer studies, pathology seemed to me the best way to understand this disease.
I met Dr. Paul Duray through two friends of mine. Barb Jones RN had been attending Lyme conferences for years because her elderly mother and her husband had severe Lyme disease, and I was a Lyme patient barely able to walk, stand or remain awake. At Lyme Disease conferences, we often spoke with Dr. Duray’s lab assistant Amy Jones and got the inside story.
When Barb’s mother died in 1994 I arranged for Dr. Paul Duray to do a brain autopsy to look for Lyme disease. Barb put $2,000 of the estate towards the cost of the research, but Dr. Duray was between jobs and institutions and to cut a long story short, the Fox Chase Cancer Center kept the money and lost the brain. I was devastated. It took over a year for them to realize they had no clue as to the location of an 87 year-old’s formalin-soaked brain!
Then in 1997 we had another opportunity to do brain Lyme research.
I had worked with three sons who had all been disabled from Lyme disease. They all made noticeable recoveries while on antibiotic therapy. The boys’ father was in a nursing home with Alzheimer’s dementia. When the family learned that their father was just a few days from dying, the oldest son wanted to do a brain autopsy to see if their father had Lyme disease just like his brothers and himself.
They all grew up on the same farm, as hunters, farmers and loggers, so their exposure to ticks was nine months a year in an area that was highly Lyme-endemic.
I urged Jim Forris to contact Dr. Alan MacDonald to do a brain autopsy. The results were stunning, confirming my suspicions and beliefs. Borrelia entered the brain and most probably caused dementia just like syphilis.
In 1997 Alan MacDonald was the first to prove by this brain-autopsy, that the Lyme bacteria not only entered the brain, but that the spirochetes penetrated neurons (nerve cells) and survived intracellularly inside human brain neurons.
This one brain-autopsy proved that Borrelia entered the brain and the spirochetes penetrated brain cells!
When the attending physician at the clinic managing Jim’s father saw the autopsy report, he spewed out that it had to be syphilis. The family was outraged so everyone in the family and the tissues were tested for syphilis. Of course all were negative and the only positive tests in the family were for Borrelia burgdorferi.

The clinic immediately got a restraining order against Jim and his family.
At the time I naively thought that the clinic would be genuinely interested in the true cause of dementia, and look into other patients’ conditions. Instead they barricaded themselves away from the truth. To my way of thinking as a scientist, this was a criminal action.
The patient had been treated previously with three rounds of doxycycline for pulmonary infections, and had sulfa drugs and metronidazole for bladder infections. So he met the IDSA criteria for proper treatment of Lyme disease, yet pathology showed his brain was positive for Borrelia in almost every cross section. This one case proved that both the tests and the treatment for Lyme Borreliosis were flawed, but not as flawed as the doctors who must diagnose Borreliosis and treat it!
——————————————————–
The association of Borrelia with brain cells in an Alzheimer’s patient was too coincidental to ignore. How was Borrelia contributing to the process of Alzheimer’s pathology?
Years later Dr. Alan MacDonald and I would team up again to try and answer that question. Only instead of waiting for people to die, Alan decided to use brain banks to get instant access to possibly infected brain tissue.
Over the years several researchers working with silver-stains had noticed that, when staining the brains of dementia patients, they would find what they thought were syphilis spirochetes. In many of the dementia brains the silver-stain would clump and form circles. Most thought this was artifact or residual stain that didn’t get washed off. Some researchers commented that they thought these clumpy circles were actually spirochetal colonies – perhaps of syphilis – and represented hundreds of spirochetes.

With today’s more accurate stains and higher resolution, we now know that these clumps were not artifacts but were “biofilms” of Borrelia, and the circles of silver-stain were probably masking the fact that the “colonies or biofilms” were covering Alzheimer plaques.
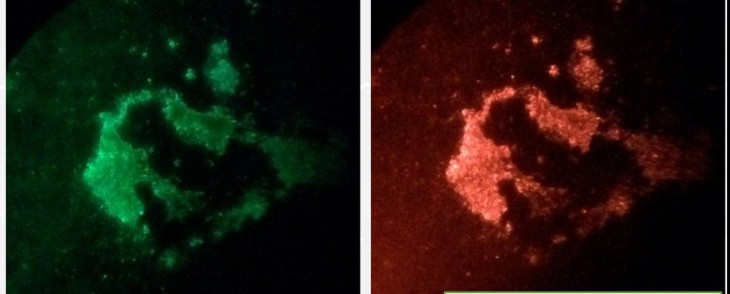
Although Alan had been doing Borrelia research for three decades, nothing propelled his research further and faster than the development of Borrelia FISH stains to allow fluorescent detection of spirochetes in human tissue.
In 2014 we had been doing our own research independently of each other and decided that we would collaborate in forming a non-profit corporation dedicated to pathology-based research. I became more administrative and Alan delved into research full force, uninhibited by bureaucracy.
We formed the Dr. Paul H. Duray Research Fellowship specifically to do the pathology-based research on Borreliosis that no one else was doing. Armed with fluorescent FISH stains for 3 different species of Borrelia, Alan took his research in new directions. (FISH, or fluorescent in situ DNA hybridization, entails finding a perfect match to a unique sequence of DNA – technology so accurate it is used to identify criminals destined to receive capital punishment.)
I would like to do an overview of the seven provocative findings of Dr. Alan MacDonald, findings that will have a positive impact on medicine for centuries.
Lyme disease is not only a fundamentally misunderstood disease: quite frankly what the public and doctors are being told by the CDC is wrong. The longer the CDC repeat the untruths despite findings that contradict them, the more their incorrect assertions have come to be seen as out-and-out lies, and purposeful misdirection.